Immune Function Testing
SPECIMEN TYPE: SERUM
Only qualified healthcare providers may order laboratory testing.
Why choose Genova Diagnostics’ Immune Function Products?
If a patient cannot quite pinpoint which foods are causing symptoms, or cannot complete an elimination challenge diet, testing can help.
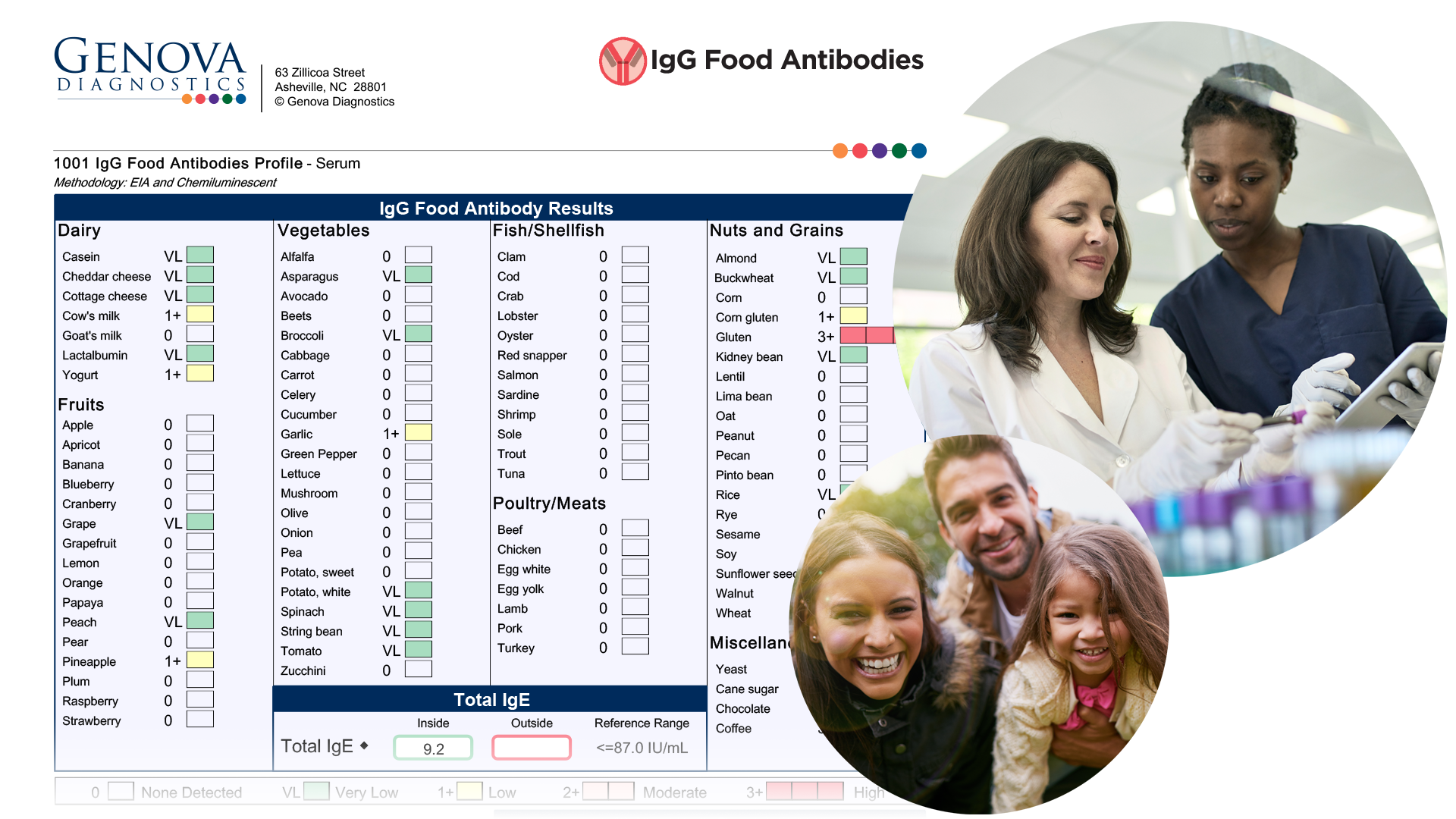
Flexible ordering allows for choosing a targeted IgG or IgE panel, or bundling several antibody profiles to give a more complete picture of the patient’s immune-mediated response.
Personalised reports list reactive/non-reactive foods to help tailor food plans.
Food and Environmental Antibody Assessment
The IgG and IgE Antibody Panels are blood tests that measure antibodies to commonly consumed foods and environmental allergens. The body can react to foods in many different ways. Adverse food reactions can lead to distressing symptoms and chronic health conditions. Often times it is unknown exactly which food(s) may be the cause and testing can help identify the problematic foods. Removal of the reactive foods often results in resolution of symptoms.
What is the difference between IgE and IgG-mediated reactions?
The key differences between IgE allergies and IgG sensitivities are summarised below:[1]
IgE-Mediated Allergies (Foods, moulds, inhalants)
- Immediate onset (minutes to hours)
- Circulating half-life of 1-2 days
- Permanent allergies
- Mast cell activation
- Stimulates histamine release
- Hives, stuffy or itchy nose, sneezing, itchy, teary eyes, vomiting, stomach cramps or diarrhoea, angioedema or swelling, shortness of breath or wheezing, anaphylaxis
IgG-Mediated Sensitivities (Foods, spices, vegetarian foods)
- Delayed onset (hours to days)
- Circulating half-life of 22-96 days
- Temporary sensitivities
- Activates complement and forms immune complexes
- Does not stimulate histamine release
- Gastrointestinal symptoms, headaches, joint aches, skin rashes, fatigue, behavioral problems, other vague symptoms
The role of IgG food antibody testing is still being researched, however studies have shown benefit of testing in certain conditions.[1] A study comparing methodologies showed that, “IgG ELISA testing is more reliable and consistent than cell size testing for identifying food sensitivities.”[21] Examples of cell size testing, or cytotoxic testing include mediator release testing (MRT), antigen leukocyte antibody testing (ALCAT) and lymphocyte response assays. These and other methodologies require well-designed trials for validation.[1]
Conditions associated with IgG food sensitivity
- Irritable Bowel Syndrome (IBS)[2,3,4]
- Major Depressive Disorder[4]
- Migraine headaches[5,6,7]
- Skin rashes such as eczema[8]
- Joint aches[9]
- Autoimmune disease[10]
- Crohn’s Disease[11]
- Obesity[12]
The “Leaky Gut” Connection
The presence of circulating IgG antibodies to foods may be suggestive of increased intestinal permeability, also referred to as “leaky gut syndrome.” When the tight junctions forming the barrier in the gut don’t work properly, larger substances can “leak” through, causing an immune response. This immune response may result in the production of IgG antibodies to foods.[4] There are multiple dietary and lifestyle factors that contribute to increased intestinal permeability. These factors include alcohol,[13] stress,[14,15] chronic NSAID use,[16] Western-type diet (high consumption of red meat, animal fat, high sugar and low fiber food),[17] and prolonged and strenuous exercise.[18,19,20]
Ordering the Profile
The Antibody Panels can be ordered as stand-alone profiles or ordered together with other profiles. Often times, clinicians will order several smaller profiles together in order to see a more complete picture of the patient’s immune-mediated response. Profiles that can be ordered together include:
- IgG Foods – 87 foods plus total IgE
- IgG Vegetarian – 21 foods plus total IgE
- IgG Spices – 24 spices plus total IgE
- IgE Food Antibodies – 19 foods plus total IgE
- IgE Moulds – 15 moulds plus total IgE
- IgE Inhalants – 25 inhalants specific to the UK plus total IgE
- Coeliac Profile – Total IgA, tTG IgA & IgG, DGP IgA & IgG, EMA IgA
Genova’s antibody testing helps to identify the body’s immune response to foods and environmental triggers with a simple blood draw.
- Some symptoms happen immediately after eating that food, while others may be delayed by several hours or days. It can be challenging to connect these delayed food reactions back to the problematic food; testing can help uncover these “hidden” food sensitivities.
There are many diverse symptoms and conditions that can result from food reactions:
- Gut symptoms such as diarrhoea, gas, constipation, cramps, vomiting, etc.
- Irritable Bowel Syndrome (IBS)
- Allergic symptoms such as sneezing, itchy eyes, sinus pain, wheezing, etc.
- Depression
- Migraine headaches
- Skin rashes such as eczema or hives
- Joint aches
- Autoimmune disease
- Crohn’s Disease
- Obesity
Every food test comes with a personalised summary of reactive foods. This can help your provider develop a tailored food plan specific to your needs and symptoms.
We have many resources to help make your testing experience a success. Review the Test Preparation tab to learn more about the collection process.
Preparing for this Test
Medications May Impact Results
Certain medications may impact test results. Please note that the reference ranges were established based on patients taking no medications or supplements. In some instances, it is unknown what potential impact a medication may have on test results. Genova never recommends that patients discontinue medically necessary medications or supplements in order to complete testing. There may be times when a patient may stay on a medication or dietary supplement during testing in order to evaluate its effectiveness. The recommendation to discontinue any substance is intended to establish a baseline finding. If you choose to discontinue a medication, a good rule of thumb is to take the biological half-life of the drug times 5 to allow for ‘clearance’ before testing. With certain medications, the drug itself may have cleared the body, but the effect of the medication may be longer lasting.
The following medications MAY INFLUENCE the antibody test results; they would not be expected to interfere with the ability to run the assay itself:
- glucocorticoids (e.g., oral prednisone, steroid metered-dose inhaler, cortisone cream)
- chemotherapy
- other immunosuppressive agents (e.g., Humira, Rituxan)
- NSAIDS (e.g., Ibuprofen, Naproxen, Aspirin)
- anticonvulsants (e.g., Carbamazepine, Valproate)
These medications can either increase or decrease immunoglobulin levels and may result in false positive or false negative test results. Omalizumab is a monoclonal antibody designed to bind to free serum IgE, which may influence test results. Heparin interferes with the measurement of tissue transglutaminase (tTG) antibodies on the coeliac panel.
The following medications DO NOT interfere with testing or influence biomarker levels: antibiotics, antihistamines, antidepressants. Antihistamines and antidepressants are known to interfere with skin prick testing, not blood testing for allergies.
Clinicians may use the allergen-specific IgE antibody test to monitor response to immunotherapy (desensitisation).
Length of Exposure to Antigens
Important: If a patient has a known IgE-mediated food allergy, Genova DOES NOT recommend exposure to the food that may cause a reaction.
When testing for food antibodies, it is suggested that the patient eat a variety of foods for 2-3 weeks prior to testing (except for foods that are known to cause severe reactions). Doing so will help to ensure the presence of antibodies to problematic foods.
It is also important to remember that IgE antibodies have a circulating half-life of 1-5 days, so any reaction shows current exposure to the antigen, meaning exposure within the several days immediately prior to collecting the test sample. The circulating half-life of IgG is approximately 21-24 days, which means that by approximately 3 months, antibodies to a particular food may be absent if the food has not been consumed by the patient. In other words, if the patient has not consumed the food prior to testing, no reaction to that food would be expected.
When running the Coeliac Profile, it is important to note that antibodies will only be present if the patient has consumed gluten prior to testing. If the patient is already on a gluten-free diet, genetic testing of the HLA DQ2/DQ8 genes may be helpful. According to the American College of Gastroenterology, a proposed gluten challenge after being gluten-free involves eating 3 grams of gluten daily for 8 weeks prior to testing. However, diagnostic changes are seen in most coeliac disease patients after as little as 2 weeks of gluten ingestion.1
Paediatric Testing
It is recommended that a child be at least 1 year old before testing for IgG antibodies in order to eliminate the possibility of maternal antibodies influencing the results. Studies are lacking on the transfer of food-specific antibodies and/or the clinical significance of these maternal antibodies measured in the child’s serum.
IgE antibodies do not cross the placenta, so there is no age restriction for IgE testing. According to Medscape, “For immunoglobulin (Ig) E-mediated allergy, there is no minimum age for testing, although it is important to consider age-related changes in patterns of sensitisation. Sensitisation to foods can occur in babies who are only a few weeks old. On contrast, it is unusual to develop sensitisation to respiratory allergens before 2 or 3 years of age. Furthermore, in preschoolers, sensitisation to indoor allergens (e.g., cat, dog, dust mites) is more common than sensitisation to pollens. Considering these patterns, it is certainly reasonable to test children for food-specific IgE in early infancy if the history suggests food allergy.”2
Breastfeeding can result in the transfer of maternal IgG and IgA antibodies to the child. However, studies are lacking on the transfer of food-specific antibodies and/or the clinical significance of these maternal antibodies measured in the child’s serum.
The immune system continues to develop into childhood. Therefore, the clinical applicability of test results in pediatric patients may be unclear. What may be interpreted as an abnormal result for an adult, may be normal for an infant’s developing immune system. This can be the case with other immune testing, including stool calprotectin and stool eosinophil protein X (EPX), where elevations would be expected in a healthy infant, but abnormal in an adult.
Diseases That May Affect Antibody Levels
Antibody testing may be inaccurate if the patient has liver disease, severe renal disease, protein-losing enteropathy, HIV infection, or other immunodeficiencies. In patients with selective IgA deficiency, coeliac disease testing should include the IgG antibody against tissue transglutaminase (tTG) and deamidated gliadin (DGP) since the IgA antibody may not be detected or may be very low.
Viruses such as Epstein-Barr virus (EBV), rubella, and cytomegalovirus (CMV) can be associated with lower antibody levels.
Results may be skewed in patients with rheumatological pathologies associated with the production of heterophilic antibodies, such as rheumatoid factor (RF).
Diseases associated with a false positive tissue transglutaminase (tTG) IgA antibody on the coeliac test may include type 1 diabetes, autoimmune liver disease, primary biliary cirrhosis, inflammatory bowel disease, connective tissue diseases, and HIV infection. Genetic testing of the HLA DQ2/DQ8 genes may be helpful in these patients.
References
- Rubio-Tapia A, et. al. ACG Clinical Guidelines: Diagnosis and Management of Coeliac Disease. Am J of Gastroenterol. 2013;108:656-676.
- Gern J. Allergy Testing in Children. Medscape. 2004. https://www.medscape.com/viewarticle/465526
| Collection Pack Instruction | Recommended Timeframe to Discontinue | Possible Impact on Results |
|---|---|---|
| Colonoscopy or barium enema | 4 weeks | May alter bacteria levels; 4 weeks is thought to be enough time for the intestinal flora to reestablish a baseline and for the GI tract to normalize after these procedures. |
| Antibiotics | The North American SIBO Consensus group recommends discontinuing antibiotics 4 weeks prior to testing. This may be beneficial for initial testing.1 Clinicians may choose to test shortly after cessation of antibiotic therapy to confirm eradication. | |
| Antifungals, herbal/natural antimicrobial products | 2-4 weeks | Can alter/influence bacterial composition. |
| Pepto-Bismol | Generally given as part of H.pylori treatment, Pepto-Bismol is also known to impact other bacteria.2 | |
| Laxatives, stool softeners, stool bulking agents (Ex-Lax, Colace, Metamucil, Fibercon) | 7 days | The North American SIBO Consensus group recommends discontinuing promotility drugs and laxatives 7 days prior to testing only if tolerated by the patient. A 4-week gap had previously been recommended, but the consensus group agreed that this time frame may not be practical for discontinuation.1 These substances can result in faster transit time and an earlier delivery of the lactulose substrate to the colon, resulting in a false-positive finding. If the use of laxatives normalizes transit time, continuing the medication may not be an issue. Fiber-containing agents may feed large intestine bacteria resulting in a false-positive finding. In patients who are severely constipated, it may be difficult to be off of this support for 7 days, so some clinicians may choose to discontinue at least 2-4 days prior. Other ways to help support patients with constipation include exercise, appropriate hydration, and trying to avoid foods that the patient knows aggravates constipation. |
| Antacids containing aluminum or magnesium hydroxide (For collections based in the United States, examples include Maalox liquid, Equate, Milk of Magnesia, Rolaids, Mylanta) | Certain antacids can influence transit time, which may influence test results. | |
| Diet must be limited; the only ALLOWED foods include baked or broiled chicken, fish or turkey (salt and pepper only), white bread (only), plain steamed white rice, eggs, clear chicken or beef broth (no vegetable pieces). Allowed beverages include water, plain coffee and tea (no sugar/artificial sweeteners or cream). | 24 hours before | High fiber foods or foods containing fermentable carbohydrates can be acted on by the large intestine bacteria. In order to ensure the test does not result in false positives or an elevated baseline from large intestine bacteria, the recommended diet must be followed. Clinicians may extend the diet to 48 hours for patients who are constipated. |
| Probiotics (i.e. acidophilus) | Probiotics have been shown to affect hydrogen levels on breath testing; the North American SIBO Consensus group did not reach a firm position statement on stopping probiotics prior to breath testing.1 | |
| Fast from food, only water is allowed | 12 hours before | Fasting prior to breath collection is important to ensure that the small intestine is clear of any food. A false positive or elevated baseline may result from not adhering to this instruction. |
| No non-essential medications or supplements, gum, candy or mouthwash | May result in elevated breath gas levels and possibly false-positive results. | |
| No smoking (including secondhand), sleeping, or vigorous exercise; this includes waiting at least 1 hour after waking for the day | 1 hour before and during | Results in elevated breath gas levels and possibly false-positive results.1 |
| Toothpaste | Toothpaste may contain fermentable ingredients for oral bacteria, resulting in a false-positive test result. |
We do not suggest collecting during an acute gastrointestinal infectious illness. Transit time and intestinal flora may be altered, which can impact test results.
Patients with Lactose Intolerance or Allergy to Lactulose
This test uses lactulose as its testing agent, and is not recommend for individuals who have had allergic reactions to lactulose, or are on a galactose/lactose-restricted diet. The full dose of lactulose for this test is 10 grams. Allergic reactions to lactulose, which are IgE-mediated and may present with such symptoms as hives, difficulty breathing, or swelling, are quite rare but can be serious. More commonly individuals may have a food sensitivity, which involves a milder, delayed reaction, which can include various symptoms including congestion, gastrointestinal discomfort, and eczema. It is also worth noting that the lactose intolerance precaution refers to those individuals who may simply have symptoms of bloating or discomfort after consuming lactose due to lactase enzyme deficiency. Though not likely dangerous, GI distress is possible with exposure to this drink in these individuals. Lactose intolerance will not interfere with test results. The healthcare provider will need to decide whether to run the test in light of a possible symptomatic response.
Patients with Diabetes
The test uses lactulose as its testing agent, and should be used with caution in diabetics, as it has the potential to raise blood sugar. Per the VistaPharm, Inc. lactulose package information,3 “since lactulose solution contains galactose and lactose it should be used with caution in diabetics.”
Transit Time
The normal transit time of lactulose (10 g) in healthy fasting patients, from the mouth to the junction between the small and large intestine (oro-cecal transit time, or OCTT), is approximately 90 minutes. In general, transit times have been found to vary in humans. Given such findings, transit time should be taken into consideration when interpreting breath testing. Substances meant to alter transit time, such as laxatives or prokinetics, should be discontinued 7 days prior to testing. If the patient is constipated, the clinician may extend the length of the limited diet prior to testing, from 24 hours to 48 hours.
Special Instructions for Patients Weighing 100 Pounds or Less/ Paediatric Patients
Follow the instructions on the blue bag for rolling and stapling the bag in accordance with weight. (Note: stapling will not damage the bag or affect the results.) This ensures that air is being collected from the appropriate part of the lungs.
According to Quintron, the manufacturer of the SIBO collection kit, the test is not appropriate for children under 25 pounds. Much of the testing requires strict adherence to collection instructions, which can be a challenge in pediatrics. There is also a strict dietary restriction in the 24 hours prior to testing regarding avoidance of certain foods that may alter the results of the test. It is required that a patient completely fast, with the exception of drinking water, in the 12 hours prior to testing. This may not be amenable in very small children. The package instructions direct the patient to stir the 10 grams (15ml or 3.3g/5ML) of lactulose solution in 8 ounces/240ml of water and drink that solution within 5 minutes after the baseline breath collection. There is not an adjusted dosage for children.
Additionally, bowel frequency and the pediatric microbiome change drastically in the first few years of life. Because of this, research is still developing on how this drastic change may influence the potential development of SIBO, as well as the most effective means to evaluate and diagnose this population. A gold standard testing option for the evaluation of bacterial overgrowth in pediatric populations has yet to be established. However, there is some literature to suggest using breath test measurement to evaluate SIBO in pediatrics.4
If a patient is not a good candidate for taking the SIBO breath test, you may consider utilising the GI Effects Comprehensive stool profile or the Comprehensive Digestive Stool Analysis 2.0 stool profile to glean information about the GI tract. Although these tests are not diagnostic for SIBO, certain biomarkers may suggest SIBO.
REFERENCES
- Rezaie A, Buresi M, Lembo A, et al. Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus. Am J Gastroenterol. May 2017;112(5):775-784.
- Pitz AM, Park GW, Lee D, et. al. Antimicrobial Activity of Bismuth Subsalicylate on Clostridium difficile, Escherichia coli O157:H7, Norovirus, and Other Common Enteric Pathogens. Gut Microbes. 2015;6(2):93-100.
- DailyMed Lactulose. National Institutes of Health U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=7016bd71-c667-46fc-8c56-5023682e8bbe
- Malik BA, Xie YY, Wine E, Huynh H. Diagnosis and Pharmacological Management of Small Intestinal Bacterial Overgrowth in Children with Intestinal Failure. Can J Gastroenterol. 2011;25(1):41-45.
Support Materials
-
Collection Instructions
Sample Reports
- Food Sensitivity+ Sample Report
- IgE Food Antibodies Sample Report
- IgE Inhalants Sample Report
- IgE Moulds Sample Report
- IgG Food Antibodies Sample Report
- IgG Spice Sample Report
- IgG Vegetarian Food Sample Report
- Coeliac Profile
Support Guide
How it Works
Consult Healthcare Provider
Your provider will discuss your symptoms and help decide which test is right for you.
Many specimen collections can be completed from the privacy of your home.
Collect Samples
Use a calendar to plan for your collection.
Follow instructions carefully and be sure to add important details about you and your specimens where indicated.
Ship to Lab
Ship specimens using the materials provided.
Schedule time with your healthcare provider to review results and create a plan for your health.
FAQ
- Review information on the Test Preparation tab above for details on how medications and supplements may impact this test.
- Support guides, charts, and additional aids can be found on the Support Materials tab. Additional educational materials can be found in our Learning Library.
RELATED PRODUCTS
Looking for added insight?
Symptoms of conditions can overlap. Certain disease states can influence other body systems. Additional testing can help identify those abnormalities.

The GI Effects® Comprehensive Stool Profile provides valuable insight into digestive function, intestinal inflammation, and the intestinal microbiome.

SIBO (Small Intestinal Bacterial Overgrowth) breath testing assesses hydrogen and methane gases to evaluate for SIBO or intestinal methanogen overgrowth (IMO).